General medicine case-05
August 24, 2022
Hello, I am p.aishwarya, a 3rd semester medical student. This is an online elog book to discuss our patients health data after taking his/her consent. This also reflects my patient centered online learning portfolio.
CASE SCENARIO:
CASE SHEET:
A 31year old man came to casuality with cheif complaints of shortness of breath since 15days and abdominal distention since 20days
CHIEF COMPLAINTS:
Case of
- SOB since 15 days
- abdominal distention since 20dayss
HISTORY OF PRESENT ILLNESS:
Patient was discharged 5days back with medication from our hospital after that he was on medication for 5 days and stopped 2days back. Decreased appetite and food intake since 2days.Distention decreased after motion and increased on eating.He has taken alcohol(2beers) and whiskey and ate chocolate .And he had cough dry cough and took medication from pharmacy.He had fever 2days ago which relieved on medication.
ASSOCIATED DISEASES:
———
PAST HISTORY:
-not a known case of HTN/DM/Asthama/epilepsy.
PERSONAL HISTORY:
Decreased appetite
Regular Bowel movements.
Has normal micturition with no burning sensation.
Has no known allergies.
FAMILY HISTORY:
Has no history of Diabetes Mellitus, No HTN, No Cardiac Strokes, No cancer.
GENERAL EXAMINATION:
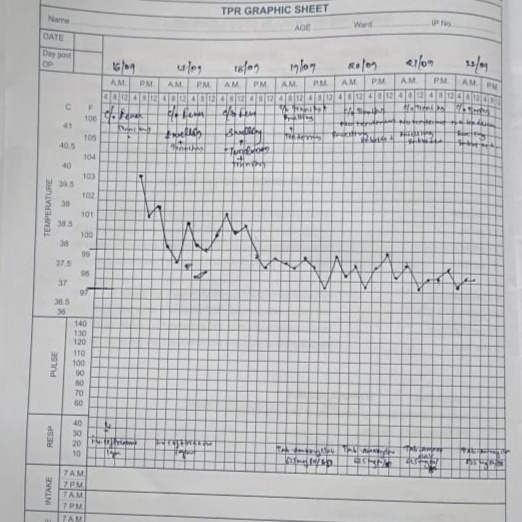
Pulse rate : 116 per minute
Respiratory rate : 20/min
B.p:110/60
Spo :90%
GRBS:157mg%
No pallor
No Cyanosis
No lymphadenopathy
SYSTEMIC EXAMINATION:
CVS
NO thrills
S1 ,S2 present
PA: soft tender
RESPIRATORY SYSTEM:
NO dyspenoea
No wheezing
Central position of trachea
ABDOMEN:
Abdomen-scaphoid
No palpable mass
No hernial orifices
No bruits
No free fluids
Bowel sounds heard
No palpable liver and spleen
CNS:
Patient is Alert
speech: normal
No neck stiffness
BIOCHEMICAL INVESTIGATIONS:
PROVISIONAL DIAGNOSIS:
Chronic liver failure